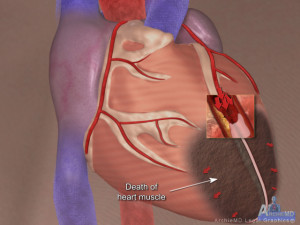
Importance of ST-Segment Monitoring Post- Acute Myocardial Infarction
When reviewing a chest pain case that has resulted in a diagnosis of Acute Myocardial Infarction it is important to ascertain if the patients ST-segment was monitored post intervention. The following are the indications for ST-Segment monitoring post-Acute Myocardial Infarction:
- Evaluating post-MI ischemia
- Evaluating reocclusion after angioplasty or atherectomy.
- Evaluating reperfusion after thrombolytic therapy.
The expected practice, as put forth by the AACN (American Association of Critical Care Nurses), is that, if available, continuous ST-segment monitoring should be performed in all 12 leads. This may not be practical in many instances, although many bedside monitors now have the capability to do this. If a continuous 12 lead is not available then the most appropriate leads should be used taking in to account the area of the patients’ infarct. This is considered the patients ST fingerprint. Many nurses monitor patients in lead II. This lead is great for arrhythmia detection but is not optimal for picking up ischemia. If the patients ST fingerprint is known then the following are the leads that should be monitored for ST-Segment elevation.
Inferior Infarct (involves the right coronary artery)
- Leads II, III, AVF
Lateral Wall Infarct (involves the left circumflex artery)
- Leads I, AVL, V5, V6
Anterior Wall Infarct (involves the left anterior descending branch of the left coronary artery)
- Leads V3, V4
Septal Infarct (involves the intraventricular septum)
- Leads V1, V2
Placement of ECG electrodes is very important and should be done with great care. The patient should be lying flat (if possible) and the nurse should actively count the rib spacing in order to place the electrodes in the proper place. You should mark the placement of the electrodes with ink that will not come off easily. The reason for this is so when the electrodes are removed for any reason they will be placed back in the exact same place. Moving the position of the electrodes can cause false positive ST-segment changes. The ST-segment alarm parameter should be set to 1 to 2 mm above and below the patient’s baseline ST segment and measure ST-segment changes 60 ms beyond the J point of the ECG complex. The J point is where the QRS meets the ST wave. ST-segment elevation or depression that last for more than one minute should be reported to the physician.
The importance of monitoring ST-segment elevation is to detect silent ischemia. It has been shown that the ECG will report ischemia before the patient clinically has symptoms.
The American Association of Critical-Care Nurses (AACN) has published two practice alerts to define the best practices for monitoring patients for dysrhythmias and ST-segment changes. (Deborah W. Kumar, 2008)
If you have a case where there were complications following an acute myocardial infarction review the records and determine if ST-segment monitoring was done and if the correct leads were utilized.
If you have a case involving an Acute Myocardial Infarction Alvin & Associates, Legal Nurse Consultants would be happy to assist you with a review of your case. Carol was involved in setting up the protocol, in the CVICU of her hospital in 2010, for ST-segment monitoring for post AMI patients. She also wrote the educational piece for this for the staff.
Works Cited
Deborah W. Kumar, R. C. (2008, Spring). Cardiac monitoring: New trends and capabilities . Retrieved August 12, 2013, from Lippincott Nursing Center: http://www.nursingcenter.com/lnc/pdfjournal?AID=776902&an=00152193-200803001-00001&Journal_ID=&Issue_ID=
Jennifer Schon
Thank you for this information; I appreciate the thoroughness and significance.