Inferior Myocardial Infarction Complications
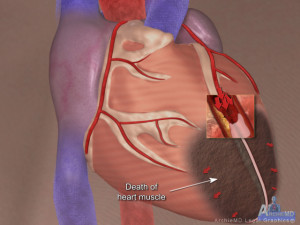
When reviewing a case involving chest pain and a resultant diagnosis of Acute Myocardial Infarction an attorney should pay particular attention to the type/area of myocardial infarction the patient sustained. An acute Inferior Myocardial Infarction has certain characteristics that set it apart from other infarcts. While the Inferior Myocardial Infarction itself, in the long run, is more benign than the Anterior or Lateral Wall Myocardial Infarction, early in the treatment of patients with these type of infarctions require highly skilled and attentive health care providers due to complications each of which can be deadly. These complications are easily treated and thus rendered harmless if recognized and treated immediately (Jay Bitar, 2010).
Early, potentially fatal (if not treated immediately), complications occurring with the Inferior Myocardial Infarction:
- Recurrent ventricular tachycardia/fibrillation – treatment includes defibrillation and anti-arrhythmic medications.
- Heart blocks – treatment includes temporary pacing.
- Bradycardia (low heart rate) – treatment includes the use of Dopamine.
- Hypotension (low blood pressure) – treatment includes the use of IV fluids.
In reviewing a case where the patient has complications/death after being diagnosed with an Acute Inferior Myocardial Infarction one should determine if, prior to going to the cath lab for an intervention, the following was performed or made readily available:
- Right – sided EKG.
- Defibrillator present.
- Access for a temporary pacemaker being utilized.

- IV fluids infused to fill the tank so to speak.
- Dopamine readily available.
Right Ventricular Infarction
Any patient that presents with a diagnosed Acute Inferior Wall Myocardial Infarction should be assessed early in treatment for the presence of a right ventricular infarct. Recognition of the syndrome of Right Ventricular Infarct is important as it defines a significant clinical entity, which is associated with considerable immediate morbidity and mortality, and has a well-delineated set of priorities for its management (SHOWKAT A. HAJI & Movahed, MD, FACP, FACC, 2000).
When reviewing the medical records of a patient diagnosed with an Acute Inferior MI look for the following clinical presentation:
- Hypotension (low blood pressure).
- Elevated Jugular Venous Pulse (JVP).
- Clear lung sounds.
- Was a right-side EKG performed?
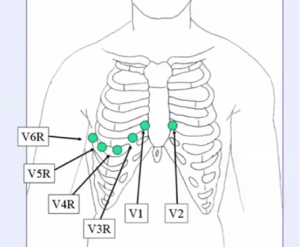
- In the presence of a Right Ventricular Infarct one would see ST-elevation in the right precordial leads V4R.
When reviewing the medical records of a patient that has been diagnosed with a Right Ventricular Infarct determine if the following treatment was provided:
- Volume loading to maintain adequate right ventricular preload (amount of volume available to the right ventricle).
- Ionotropic support (pressor medications for supporting low blood pressure).
- Maintenance of atrioventricular synchrony (heart activation sequence in which first the atria then – after an appropriate delay – the ventricles contract). This may require a temporary pacemaker.
In summary, a patient presenting with chest pain, that is diagnosed with an Inferior Wall Myocardial Infarction, has a condition, if treated immediately and appropriately, should in the long term, provide less damage than an Anterior Wall Myocardial Infarction. But this condition does have early, potentially fatal complications that can lead to death if the patient does not undergo the appropriate diagnostic testing and receive the appropriate treatment.
Works Cited
Jay Bitar, M. F. (2010, November). Teasing Death in Acute Inferior Infarct. Retrieved from Cath Lab Digest: http://www.cathlabdigest.com/articles/Teasing-Death-Acute-Inferior-Infarct
SHOWKAT A. HAJI, M., & Movahed, MD, FACP, FACC, A. (2000). Right Ventricular Infarction—Diagnosis and Treatment. Clinical Cardiology, 473-482.
Leave a Comment