A percutaneous coronary intervention (PCI) is often called balloon angioplasty. A catheter is inserted into the blood vessels either in the groin (femoral artery) or in the arm (radial artery). Using a special type of X-ray called fluoroscopy; the catheter is threaded through the blood vessels into the heart where the coronary artery is narrowed. When the tip is in place, a balloon tip covered with a stent is inflated. The balloon tip compresses the plaque and expands the stent. Once the plaque is compressed and the stent is in place, the balloon is deflated and withdrawn. The stent stays in the artery, holding it open (Percutaneous coronary intervention–PCI or angioplasty with stent, 2012). 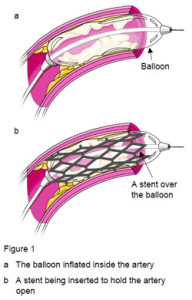
The focus of this blog post will be the standard of care required of nurses caring for patients immediately post PCI.
PCI is an invasive procedure that carries with it significant risks that nurses need to be aware of when caring for these patients. Several factors can influence the risk of developing vascular complications during or after cardiac catheterization. These include patient characteristics, the interventional cardiologist’s technique, medications used during catheterization, the use of manual or mechanical compression at the access site, the use of closure devices, and the quality of nursing care (Charlotte Huber, August 2009).
Potent antithrombotic agents and regimens are used prior to and during the PCI which may increase the effectiveness of percutaneous coronary intervention, they are also generally associated with an increased risk of vascular access complications such as hematoma, retroperitoneal hematoma, pseudoaneurysm, arterial occlusion, and arteriovenous fistula, which in turn are associated with increased morbidity, mortality, and costs. Risk factors predisposing patients to these complications are both modifiable (procedure technique, medications, hemostasis method) and nonmodifiable (sex, age, body mass index, blood pressure, renal function). Patients’ risks can be reduced by nurses who are knowledgeable about these risk factors and identify complications before they become problematic (Nakia Merriweather & Sulzbach-Hoke, RN, PhD, CCNS, ACNS-BC, CCRN, October 2012).
Nursing care of the patient post PCI procedure may occur in different settings including, intensive care unit, cath lab recovery, and in some hospitals a medical floor. Upon receiving the patient from the cath lab it is important for the nurse that will be taking care of the patient to obtain a comprehensive report that includes: medications given during the procedure, stents placed and their location, time of last heparin dose (if given), number of sticks required to place the sheath (this is very important), most recent vital signs, visualization of the sheath site with the cath lab nurse, and assessment of pedal pulses.
Prior to removing the sheath, unless the patient has received Angiomax (anticoagulant), generally orders are written for ACT’s (activated clotting time) to be drawn until the level is generally less than 150. It should be noted that in patients that have received Angiomax ACT levels do not decrease and generally the physician orders will note when the sheath should be pulled. Units caring for these patients should have protocols in place for the care of these patients prior to the sheath being pulled, for the sheath pull procedure itself, and then post sheath pull. These protocols will address frequency of vital signs and assessment of the sheath site and pedal pulses, positioning of the patient, and systolic blood pressure levels that need to be addressed prior to pulling sheaths. The following protocol was in place when I was part of the sheath pull team in my CVICU:
• Vital signs, site assessment, and pedal pulse checks every 5 minutes x 3, every 15 minutes x 2, and then every ½ hour until the sheath is removed.
• Head of bed at 30 degrees or less. If bleeding occurred or presence of hematoma then lie the patient flat.
• Atropine to be at the bedside for sheath pull (pressure applied during sheath pull my cause vagal response and decreased heart rate).
• 2 staff required at the bedside during sheath pulls.
• The RN pulling the sheath should have received formal training and performed a requisite number of observed sheath pulls prior to being in charge of a sheath pull procedure.
• Sterile gloves and masks to be worn during procedure.
• Supplies required for procedure: sterile towels, sterile scissor for cutting suture, sterile gauze, and sterile transparent dressing for post sheath pull to cover insertion site.
• Fluid infusing during procedure.
• Vital signs and pedal pulse check every 5 minutes during sheath pull.
• Documentation of sheath pull procedure should include whether or not the sheath was intact, presence of hematoma pre- or post-sheath pull, presence of hemostasis post sheath pull, and how patient tolerated the procedure.

In the event that you are a Legal Nurse Consultant reviewing a case that involved a patient that underwent a PCI procedure it would be important to have the attorney request from the hospital educational files related to sheath pull education and certification for the unit involved and the policy and procedure for sheath pulls.
The next blog post will address the complications that may occur post PCI procedure.
If you are an attorney that has a case involving any PCI procedure or other heart related matter please consider contacting Alvin & Associates to help you review the medical aspects of your case. Carol received her certification in Cardiac Medicine in 2010 from the American Association of Critical Care Nurses.
Alvin & Associates, Legal Nurse Consultants
http://www.alvinandassociatesLNC.com
Works Cited
Charlotte Huber, M. R. (August 2009). Safety After Cardiac Catheterization–Minimizing vascular complications. AJN, 57-58.
Nakia Merriweather, R. M., & Sulzbach-Hoke, RN, PhD, CCNS, ACNS-BC, CCRN, L. M. (October 2012). Managing Risk of Complications at Femoral Vascular Access Sites in Percutaneous Coronary Intervention. Critical Care Nurse, 16-30.
Percutaneous coronary intervention (PCI or angioplasty with stent). (2012, June). Retrieved April 27, 2014, from Heart and Stroke Foundation: http://www.heartandstroke.com/site/c.ikIQLcMWJtE/b.3831925/k.4F32/Heart_disease__Percutaneous_coronary_intervention_PCI_or_angioplasty_with_stent.htm
lynne b woodside AS RN CLNC
Thanks a heap! I had this very procedure performed a year ago – and I found this VERY interesting- and helpful. My PCI was an emergency (as in Life or Death), I’m told – and “my” team were champions! Again – thanks!