In October 2002, on the basis of published evidence, the Advanced Life Support Task Force of the International Liaison Committee on Resuscitation made the following recommendation:
Unconscious adult patients with spontaneous circulation after out-of-hospital cardiac arrest should be cooled to 32°C to 34°C for 12 to 24 hours when the initial rhythm was ventricular fibrillation (VF).
Such cooling may also be beneficial for other rhythms or in-hospital cardiac arrest (J.P. Nolan, Morley, MD, Vanden Hoek, MD, & Hickey, MD, 2003).
Induction of hypothermia after return of spontaneous circulation post cardiac arrest has been found to positively affect functional recovery and reduce cerebral deficits.
Approximately 300,000 people in the United States suffer out-of-hospital cardiac arrest per year. Despite Advanced Cardiac Life Support, the survival rate of out-of-hospital cardiac arrests is very poor. Less than half of the people who have a return of spontaneous circulation survive to leave the hospital alive and the cause of death in most of these patients is anoxic brain injury. Inducing mild therapeutic hypothermia in selected patients surviving out-of-hospital sudden cardiac arrest has a major impact on long-term neurologically intact survival and may prove to be one of the most important clinical advancements in the science of resuscitation (Therapeutic Hypothermia , 2013).
Despite its 2005 inclusion in American Heart Association Guidelines for CPR and Emergency Cardiovascular Care hypothermia therapy is largely misunderstood and inconsistently applied (Therapeutic Hypothermia , 2013).
Implementation of hypothermia does require planning, education, and integration of multiple services within an institution.
The American Heart Association has requirements that should be met for a patient to undergo the hypothermia protocol. These include:
- Full code status prior to arrest
- Motor score in the Glascow Coma Scale <6
- No alternative reason for coma
- Pre-arrest neurological status not meaningfully impaired
- Hemodynamically stable; no uncontrolled dysrhythmias
- No uncontrolled bleeding
- Absence of multi-organ dysfunction or sepsis
- ?Prolonged arrest time (>60 minutes)
Exclusions:
- Traumatic arrest
- Actual or uncontrolled bleeding
- Pregnancy
- Cardiac instability
- Uncontrolled hypotension—MAP<70 despite vasopressors
- Pre-existing environmental hypothermia
In most centers, the patient is actively cooled by using an induced hypothermia protocol for 24 hours to a goal temperature of 32-34ºC. The goal is to achieve the target temperature as quickly as possible. In most cases, this can be achieved within 3-4 hours of initiating cooling. Rewarming is begun 24 hours after the time of initiation of cooling (ie, NOT from the time the target temperature is achieved) (Therapeutic Hypothermia , 2013).
When trying to achieve a hypothermic state shivering is usually a concern. Shivering is not only uncomfortable but produces heat which interferes with the cooling process. Usually sedation and paralysis are necessary during the cooling phase. Medications used for sedation often use medications from the following list: fentanyl/lorazepam or /midazolam or propofol. To achieve paralysis cisatracurium is often used. Demerol may be used to decrease the shivering threshold. The train-of-four is often part of the protocol for assessing the level of paralysis when using a paralytic but this device may not function properly when the patient is cold.
Cooling must be performed rapidly to achieve maximum effectiveness and should be instituted as early as possible. Most studies have found it necessary to use both cooling blankets and ice packs to achieve the temperature goal. Other methods such as ice lavage, cold saline infusion, and endovascular methods may be used to help achieve target temperature (Therapeutic Hypothermia , 2013). 2 liters of cooled saline is often instilled initially as part of the protocol.
A continuous core temperature monitor should be used; this provides data to modulate cooling efforts and to avoid overcooling. One method of doing this is to use a pulmonary artery temperature probe. A secondary method for monitoring the temperature should be used. This can be a bladder temperature or esophageal. Bladder temperatures require adequate urine output.
Complications of the Hypothermia Protocol:
- Coagulopathy
- Arrhythmias
- Hyperglycemia
- Unintended drop of temperature below target
- Likelihood of pneumonia and sepsis may increase
- Hyperthermia is common after resuscitation; this can impair brain recovery (2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science, 2010).
Goals During the Hypothermia Protocol:
- Temp 32 – 340 C for 24 hours
- MAP 80 – 100 (may be lower in ACS) controlled
with pressors (norepinephrine/epinephrine),
inotropes – ejection fraction-dependent
(dobutamine), nitroglycerin, esmolol
- CVP 8 -15 (fluids)
- SVO2 >65% (fluids, blood prn)
- Decreasing lactate (2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science, 2010)
EEG should be monitored continuously during the hypothermia protocol if at all possible. Continuous EEG monitoring showing a nonreactive or discontinuous background during Therapeutic Hypothermia is strongly associated with unfavorable outcome in patients with coma after cardiac arrest (Rossetti, Urbano, Delodder, Kaplan, & Oddo, 2010).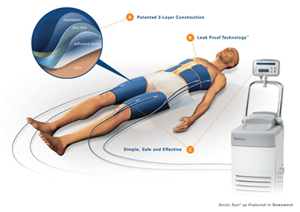
The hypothermia protocol is not difficult to institute but careful attention needs to be made to not over-cool the patient. Attention to possible adverse effects is necessary. Hypothermia protocol helps save cardiac arrest patients from neurological deficits and is an important part of the resuscitation and post-resuscitation care of the Cardiac Arrest patient.
Works Cited
2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science. (2010, October). Retrieved October 10, 2013, from Circulation: http://circ.ahajournals.org/content/122/18_suppl_3/S768.full
Therapeutic Hypothermia . (2013, June 19). Retrieved October 10, 2013, from Medscape: http://emedicine.medscape.com/article/812407-overview
J.P. Nolan, F., Morley, MD, P. T., Vanden Hoek, MD, T. L., & Hickey, MD, R. W. (2003, October). Therapeutic Hypothermia After Cardiac Arrest. Retrieved October 10, 2013, from Circulation: http://circ.ahajournals.org/content/108/1/118.full
Rossetti, A. O., Urbano, L. A., Delodder, F., Kaplan, P. W., & Oddo, M. (2010, October). Prognostic value of continuous EEG monitoring during therapeutic hypothermia after cardiac arrest. Retrieved October 10, 2013, from Critical Care: http://ccforum.com/content/pdf/cc9276.pdf
Leave a Comment