The nursing assessment is an important tool not only for the nurse performing the assessment but as I tool to determine progress or lack of progress of a patient. As a Legal Nurse Consultant reviewing the nursing record of a patient you also need to determine the accuracy of the assessments. One might suggest that this is not possible because they do not have the ability to know or have seen the patient at the time of the assessment. Unfortunately, in my experience as a bedside nurse and in reviewing cases, nursing assessments are not always performed as completely as the documentation would suggest. How does a Legal Nurse Consultant determine when an assessment, or any other documentation, have erroneous information? Obviously the LNC was not there at the time of the assessment but they are privy to issues that arise in the patient’s ongoing care, through review of the medical record, which can suggest that assessment documentation is flawed.
During most of the 30 years I spent as a bedside nurse in various ICU settings nursing assessment documentation was performed as a narrative. The nursing documentation forms for a 24 hours period consisted of 2 pages. One page was for the vital signs, IV fluids and other intake forms, and then various forms of output. The second page was for the every 4 hour assessments with boxes delineating out the different systems of the body, such as, cardiovascular, urinary, GU, skin, etc. The assessments were written in a narrative manner. Generally if something was not addressed it had not been assessed. I used the total narrative style type documentation form during my first 10-11 years when I was working in the SICU and to be honest I do not specifically remember an instance where I followed somebody and found that something was addressed as being assessed that obviously had not been assessed.
Next I transferred to the PACU for the next 11 years and the form was different in that in your areas of the systems you, at times, had boxes you could check to note that, for instance, heart sounds were regular, lung sounds were clear, pupils were PERRLA, patient was alert and oriented, etc. This is when I began noticing discrepancies between the assessments and the patient’s actual condition. To be honest the discrepancies generally were related to pupil assessments and heart sounds. I can remember 3 specific instances where the assessment noted that the patients’ pupils were PERRLA and I found the following: 1) the patient only had one eye, 2) the patient asked me as soon as I came on if I wanted him to remove his prosthetic eye prior to surgery or if I wanted to do so, and 3) I called the neurosurgeon on a patient that had undergone a craniotomy because his pupils were significantly unequal and the doctor got upset that I bothered him because his pupils had been like that since surgery. After I transferred to the CCU, which eventually became the CVICU, this problem with pupil assessment continued but then it had more to do with the nurses simply left that part of the assessment blank. In both instances the size of the pupils (there was a place available for that input) was left blank. So why would a nurse chart something that they had not actually done? I was baffled then as to what I thought was an anomaly and continue to be baffled when I review medical records and find that things that have been charted could not have actually been performed (obvious because of an negative outcome for a patient).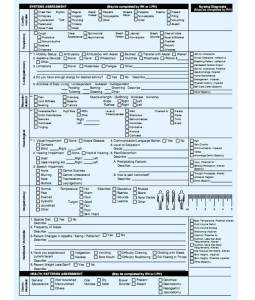
I am going to provide an actual example of a policy instituted that could have led to a negative outcome. Please note that I am unaware of any ruptured pulmonary arteries occurring in the unit during the years that I worked in the unit. We often had patients in acute exacerbated heart failure in our CVICU. Often these patient’s had Swan-ganz catheter’s in place. Chest x-rays were done on these patients’ every morning to confirm placement of the Swan-ganz catheter. The manager of our unit decided it was a nursing responsibility to read these x-rays and notify the physician if a line needed to be repositioned. First of all I personally do not think that reading x-rays is within the usual education, skill, experience and job description of a bedside nurse without advanced training. Secondly no formal training was provided for this new responsibility. I felt fortunate that I did quickly, thanks to a resident, learn to read these x-rays and often was able to point things out to the residents that they had not seen. But most of the nurses simply came to me when their x-rays came up in the morning because they were unable to read the x-rays. Now imagine if a nurse, that was unable to see that the Swan-ganz catheter in her patient had migrated in too far, simply charted (because she was afraid she would get in trouble with the manager for not being able to read the x-ray) that the Swan-ganz placement was verified by x-ray. The day shift nurse comes on and her other patient crashes and she is away from the bedside of her other patient and most everybody else is also busy with the patient that crashed. The patient with the Swan-ganz catheter, that is now in too far, suddenly has a permanent wedge tracing show up on the monitor but everybody is too busy to see this tracing. Eventually the pressure on the pulmonary artery causes the artery to rupture. Who is responsible for this breach of duty that resulted in the rupture and possible death of a patient? The bottom line is that the nurse should not have documented that the Swan-ganz catheter placement was verified. She was not able to adequately read the x-ray and therefore should have gone to a resident that would have been available in the unit, to check the placement of the Swan-ganz catheter. Hopefully he would have seen that the line had migrated in too far and pulled the catheter back.
So my question is why do nurses chart things that they actually do not do or observe? I will never know the answer to that question but unfortunately I know that this happens. When I review a medical record I keep in mind that what you see is not always what happened.
Leave a Comment