Previously the nursing care post PCI procedure was discussed focusing on what a PCI is, vital signs and monitoring of the insertion site, and removal of the sheath. This post will address the complications that can occur prior to and after sheath removal, and the interventions to take if any of these occur.
Hematoma
This is bleeding into the area surrounding the insertion site and can occur prior to and after a sheath pull. The nurse will see swelling at and around the insertion site and the patient may experience pain. Factors that can influence possible development of a hematoma include procedural factors such as a larger sheath size (greater than 8 Fr.), site of entry below the common femoral artery, multiple sticks, and excessive use of anticoagulants. Factors that can affect the formation of a hematoma that are patient driven include hypertension, female sex, a patient prone to bleeding episodes for any reason, age, obesity, and peripheral vascular disease. (Hamel, February 2009).
When a nurse observes a hematoma forming they should immediately apply pressure to the site and check the distal pulse. The physician should be notified and generally an order to draw a CBC is given. Generally serial CBC’s will be monitored after an event such as this. If the hematoma forms prior to the sheath pull the sheath needs to be removed as soon as possible.
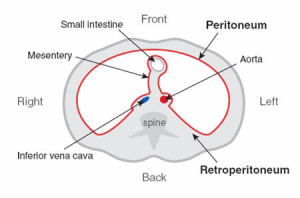
Retroperitoneal Hemorrhage
A retroperitoneal hemorrhage is bleeding into the retroperitoneal space. This can be very serious and the patient can lose a large amount of blood into the retroperitoneal space. Symptoms can include a groin hematoma; fall in hemoglobin/hematocrit, hypotension, abdominal/flank pain, nausea/vomiting, diaphoresis, flank ecchymosis, and bradycardia (Suggs, Reagan, Clements, & Hardin, January 2013). Any time a patient complains of abdominal/flank pain and starts dropping their blood pressure the nurse should immediately call a physician and get a CBC ordered. The physician will probably order a CT scan. If the patient has not been typed and crossed for blood products prior to this and the physician does not order the lab test, the nurse should suggest that this be drawn with the first CBC draw.
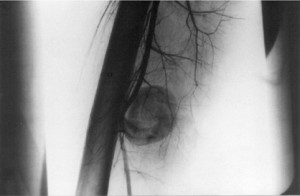
Pseudoaneurysm
Commonly a puncture of one of the weaker walls of the branch of the femoral artery, causing bleeding in the tissue surrounding the artery via a small tract and forming a wall around the artery (Hamel, February 2009). This complication can appear within12-72 hours post procedure. The clinical presentation includes auscultation of a bruit, pain, swelling, and severe bruising at the arterial puncture site. Compression therapy is appropriate for pseudoaneurysms that are less than 2cm. Ultrasound guided thrombin injection at the site is required for those that cannot be resolved with compression therapy. Femoral pseudoaneurysms may occur on up to 8% of vascular interventional procedures. A pseudoaneurysm is generally initially detected when the nurse monitors the insertion site (Suggs, Reagan, Clements, & Hardin, January 2013). Part of the nurses’ assessment should include auscultation for a bruit (a rushing or swishing type sound).
Arteriovenous Fistula
Puncture of the artery and vein causing a tract to form and allowing direct communication between them. Many of these fistulas are small and resolve spontaneously. AV fistula is often associated with a low groin puncture and can occur during manual compression. It is typically asymptomatic but can result in numbness due to a reduced flow of blood and reduced distal pulses following catheterization (Suggs, Reagan, Clements, & Hardin, January 2013).
The above complications are the most frequent complications occurring post PCI procedure and arterial sheath removal. The Legal Nurse Consultant when reviewing cases involving complications from a sheath removal should focus on the nursing documented assessment of vital signs and the site, and any interventions taken when the complication initially was noticed. Was a physician immediately notified? Were appropriate labs and radiographic studies performed? If needed, were serial CBC’s performed? Just because a physician does not place an order it does not mean that the registered nurse cannot suggest that certain labs or procedures should be done.
Works Cited
Hamel, W. J. (February 2009). Femoral Artery Closure After Cardiac Catheterization. Critical Care Nurse, 39-46.
Suggs, P. M., Reagan, S. R., Clements, F. C., & Hardin, S. R. (January 2013). Factors associated with groin complications post. Clinical Nursing Studies, 26.34.
If you are an attorney that has a case involving any PCI procedure or other heart related matter please consider contacting Alvin & Associates to help you review the medical aspects of your case. Carol received her certification in Cardiac Medicine in 2010 from the American Association of Critical Care Nurses.
Alvin & Associates, Legal Nurse Consultants
http://www.alvinandassociatesLNC.com
jane shufro
Hi Carol,
I enjoyed your articles very much. I wanted to let you know I think you are very articulate in the way you explain medical terminology and procedures. I’m a fairly new LNC bur I worked for many years in a cath lab which is why I was interested in your posts. I’m in a PACU and work part time as an independent LNC. I testify mostly in anesthesia related events. I’ll keep you in mind should I come across a cardiac case.