The discussion in this blog post will continue the discussion of Anatomy of a Chest Pain Case: What Attorneys Must Know to Navigate the Medicine, addressing the different types of Myocardial Infarction, diagnostic testing, and treatment. Please refer to the previous blog post regarding this topic for an introduction to the topic.
When a patient presents with chest pain an EKG should be performed within 10 minutes of arrival in the Emergency Department to assess for ST-segment elevation or new onset left bundle branch block (LBBB). After obtaining the EKG if the patient is suspected of having an Inferior Acute Myocardial Infarction then a Right-sided EKG should be obtained (discussed in more depth below under Treatment that should be considered). The EKG is an important diagnostic tool in that, in the presence of signs and symptoms of Acute Myocardial Infarction, the EKG will help differentiate between ST-elevated Myocardial Infarction (STEMI) and NSTEMI (Non-ST-elevated Myocardial Infarction). Serum cardiac biomarkers (CK-MB and cardiac troponins) are also important diagnostic tools used in diagnosing Acute Myocardial Infarction; but if clinical suspicion of an Acute Myocardial Infarction is high it is not necessary to wait for the results of this testing before initiating reperfusion therapy.
STEMI (ST–elevated Myocardial Infarction)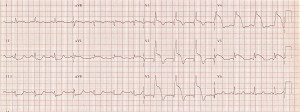
Reperfusion therapy is the most important step in the management of the patient with a ST elevated myocardial infarction as this improves the flow of blood to the site of the infarct. Every 30 minute delay to treatment increases the risk of mortality. Types of reperfusion therapy include medication in the form of fibrinolytic agents, PCI (percutaneous coronary intervention), and CABG (coronary artery bypass surgery).[1]
Choice of reperfusion technique relies on 3 factors:
- Time from onset of symptoms, as initiation of fibrinolytic therapy within 2 hours from the start of symptoms could terminate the ST-elevated Myocardial Infarction, thus decreasing the risk of death.
- Percutaneous coronary intervention is the preferred technique in patients with a bleeding risk.
- Availability of Percutaneous coronary intervention, including time needed for transfer, distance from the place of diagnosis to a percutaneous coronary intervention center, and availability of transportation.
- Time to definitive treatment should be within 30 minutes for fibrinolytic therapy and within 90 minutes for percutaneous coronary intervention. This time frame is very rigid in PCI – capable centers. In patients that require transportation to a PCI – capable center, PCI is the first option provided the time to treatment does not exceed 2 hours.
- Percutaneous coronary intervention should be performed in patients with STEMI and ischemic symptoms that have been present for less than 12 hours. It is also a reasonable therapy for patients with hemodynamic instability, severe heart failure, or persistent ischemic symptoms who present to the Emergency Department 12 – 24 hours after symptom onset.
- Coronary artery bypass surgery (CABG) is indicated in patients with STEMI and ongoing ischemia who are not candidates for either thrombolytic therapy or percutaneous coronary intervention. CABG is also considered a reasonable treatment in patients with left main stenosis of 50% or more and/or three-vessel disease.
- Patients that develop complications during percutaneous coronary intervention, the procedure was not successful, or have ongoing ischemia should undergo emergency coronary artery bypass surgery.[2]
Treatment that should be considered in addition to reperfusion therapy includes:
- Patient who will be undergoing percutaneous coronary intervention should be given antiplatelet agents such as P2Y12 receptor blockers (Clopidogrel, Ticlopidine, Cangrelor, and Prasugrel are examples) and glycoprotein IIb/IIIa inhibitors (ReoPro, Integrilin, and Aggrastat).
- Nitrates, such as nitroglycerin, for vasodilation and pain control (use cautiously in patients where there is suspicion for a right ventricular infarct).
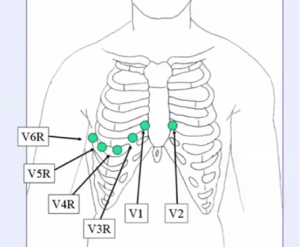
- Right-sided EKG should be obtained in patients that have an Inferior STEMI to determine if the patients has developed a Right Ventricular Infarct. If a Right Ventricular Infarct exists there will be ST-segment elevation on the right sided EKG or ST-depression in lead V2. Patient with a Right Ventricular Infarct are preload dependent (require increased levels of IV fluids) and nitrates should not be used as part of their therapy.
- ST-depression in V2 + elevation in V1 indicates the presence of a Right Ventricular Infarct; ST-depression in V2 + isoelectric ST-segments in lead V1 and V3 indicate a Right Ventricular Infarct[3]
- Morphine is the preferred treatment for pain in patients with STEMI pain.
- Beta-blockers (Atenolol, Metoprolol, and Carvedilol are examples) to decrease the heart rate and force of contraction, thus decreasing the work-load and oxygen demand on the heart.
- Anticoagulant therapy such as heparin.[4]
Once the patient has undergone reperfusion therapy the patient should be monitored closely for ST – segment elevation (this topic will be addressed more in depth in a later post), heart rhythm, and symptoms. The patient should also be monitored for signs and symptoms of hemodynamic complications secondary to the Acute Myocardial Infarction, systolic heart failure (low-output failure), cardiogenic shock, right ventricular infarction (generally found in patient with an infarct involving the right coronary artery), pulmonary edema, and arrhythmias.
ACE inhibitors (Lisinopril, Captopril, and Ramipril are examples) is given to all patients that have an anterior STEMI, heart failure, or ejection fraction </= to 40% to reduce morbidity and mortality
NSTEMI (Non ST-elevated Myocardial Infarction)
Patients that have a Non-ST-elevated Myocardial Infarction should not undergo fibrinolysis as it is not beneficial and can be harmful. These patients should undergo a conservative treatment plan with the use of medical therapies or early invasive therapy with angiography and revascularization with Percutaneous Coronary Intervention or Coronary Artery Bypass Graft Surgery. These patient should receive prompt treatment with antiplatelet and antithrombotic agents such as heparin, fondaparinux, and in patient that will be undergoing Percutaneous Coronary Intervention, bivalirudin (Angiomax).[5]
Unstable Angina
Unstable Angina and non-ST elevation myocardial infarction differ primarily in whether the ischemia is severe enough to cause sufficient myocardial damage to have cardiac biomarkers become positive, thus indicating myocardial injury. Because elevation in cardiac biomarkers are often not detectable for up to 12 hours from onset of symptoms Unstable Angina and non-ST elevation myocardial infarction are frequently indistinguishable at the time of initial evaluation.[6]
The course of unstable angina can be highly variable and potentially life-threatening; therefore a management strategy should be decided upon expeditiously. Will treatment be invasive or conservative?
Conservative management:
- Initiation of anticoagulant therapy
- Enoxaparin or unfractionated heparin
- Angiomax or fondaparinux
- Initiation of therapy with Clopidogrel.
- Consider the addition of Integrilin or tirofiban.
Invasive Treatment:
- Diagnostic Angiography[7]
Part 3 of this series will discuss post reperfusion therapy ST-segment monitoring.
The next time you are handling a medically complex case contact Alvin & Associates, Legal Nurse Consultants. We can review for merit, do chronology/timelines, and find experts for your medically related case.
[1] (Elsevier’s First Consult – Acute Myocardial Infarction)
[2] (Elsevier’s First Consult – Acute Myocardial Infarction)
[3] (Ali Farzad, 2011)
[4] (Elsevier’s First Consult – Acute Myocardial Infarction)
[5] (Elsevier’s First Consult – Acute Myocardial Infarction)
[6] (Allan S Jaffe & Morrow, MD, MPH, 2015)
[7] (Walter Tan, 2014)
Leave a Comment